Hypertension, often referred to as the silent killer, quietly undermines the health of millions worldwide. Despite its stealthy nature, the repercussions of uncontrolled high blood pressure can be catastrophic, ranging from heart disease to stroke. Therefore, managing hypertension isn’t just a short-term fix but a lifelong commitment essential for overall well-being.
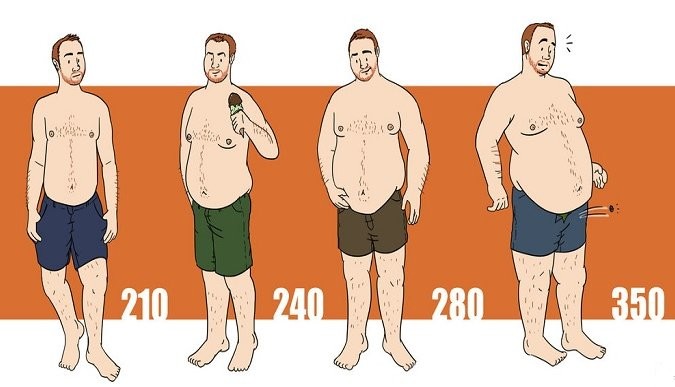
The Relationship Between Obesity and Hypertension
Obesity and hypertension share an intimate connection, forming a vicious cycle that heightens cardiovascular risk. Excess weight, particularly visceral fat around the abdomen, triggers hormonal changes, inflammation, or kidney damage, leading to high blood pressure. Recognizing this link underscores the importance of addressing obesity as a cornerstone of hypertension management.
Understanding Visceral Fat
Visceral fat, also known as intra-abdominal or belly fat, accumulates deep within the abdominal cavity, encircling vital organs such as the liver, pancreas, and intestines. Unlike subcutaneous fat, which lies just beneath the skin, visceral fat poses greater health risks due to its association with insulin resistance, diabetes, increased LDL (bad cholesterol), and hypertension.
Managing Hypertension Through Weight Loss
Shedding excess pounds isn’t just about appearances but is crucial for lowering blood pressure. Even a modest weight loss of one kilogram can reduce blood pressure by 1-2 mm Hg, subsequently lowering the risk of stroke and heart attack. Adopting dietary changes, such as the DASH (Dietary Approaches to Stop Hypertension) diet and intermittent fasting, can be instrumental in combating hypertension by promoting weight loss and improving metabolic health.
The DASH Diet and Intermittent Fasting
The DASH diet emphasizes the consumption of fruits, vegetables, lean proteins, whole grains, and healthy fats while restricting sodium intake. This balanced approach helps lower blood pressure levels by promoting potassium intake, countering the effects of sodium, and reducing LDL cholesterol. Additionally, intermittent fasting improves insulin sensitivity, reduces inflammation, aids in weight loss, and enhances fat burning, contributing to better blood pressure control.
Considerations and Consultation
Before embarking on significant dietary changes or exercise regimens, especially for individuals with existing health conditions or medication regimens, consulting with a healthcare provider or registered dietitian/qualified trainer is advisable. Long-term adherence to a balanced diet, coupled with regular exercise, is vital for sustainable blood pressure control and overall health.
In conclusion, managing hypertension is a multifaceted endeavor that requires a lifelong commitment to healthy lifestyle choices, including dietary modifications, weight management, and regular medical monitoring. By understanding the intricate relationship between obesity and hypertension and adopting evidence-based strategies, individuals can take proactive steps towards mitigating the risks associated with this silent but deadly condition.